Dark neurodivergence or Cluster B traits?
When self-diagnosed neurodivergence becomes a shield for Cluster B behaviour
We are living in a time when mental health labels have shifted from clinical tools to social identities. That shift has brought cultural visibility and compassion, but it has also blurred important lines. In today’s therapeutic and cultural climate, diagnoses like autism and ADHD have become more accessible, socially acceptable, and even desirable for some adults. These labels offer legitimacy, protection, and empathy, while Cluster B personality disorders remain steeped in stigma, often associated with moral failure rather than neurological difference.
Talking about this is, in itself, taboo. In today’s cultural climate, questioning how neurodivergence is framed, especially since it intersects with trauma, identity, or inclusion, is often met with defensiveness or accusations of ableism. We have to make room for complexity, because complexity exists and is more accurate than our artificial, reductionist categories aimed at simplifying diagnostic processes and treatment pathways, based on a specific paradigm of the human condition. We can affirm that autism and ADHD are real, often impairing neurodevelopmental conditions, and still acknowledge that some people are misusing these labels in ways that obscure deeper dysfunction, bypass personal growth, and erode trust in the systems built to support genuine disability. Avoiding the conversation does not protect those who have greater vulnerability. It protects antisocial dynamics and prioritises not hurting feelings over protecting people who are at risk of being manipulated, harmed, or dismissed in environments that mistake dysfunctional behaviour for disability.
Psychotherapist Skye Sclera’s piece explores the overlap between ADHD and narcissism, unpacking how neurodivergent traits can be misread and sometimes misused in ways that obscure both personal responsibility and relational impact.
People who express chronic manipulation, emotional volatility, or low empathy are far more likely to be tested or self-identify as neurodivergent than to be evaluated for personality dysfunction. This departure from diagnostic precision (and discernment) has blurred the line between genuine neurodevelopmental conditions and characterological disorders, and it raises questions about rigid diagnostic criteria that prioritise presentation over the socioecological and developmental influences that shape a person’s neurological and behavioural patterns. Whether intentional or not, many now adopt terms like neurodivergent, autistic, or the increasingly popular hybrid label AuDHD because these frameworks match their internal experience and offer a sense of clarity or relief. However, in practice, these labels can function as moral shields that deflect scrutiny, interpret harmful behaviour as misunderstood difference or personality clash, and grant a kind of instant immunity from accountability, especially in workplaces that rigidly adhere to DEI policies and seek to avoid the reputational risk of appearing discriminatory.
In this piece, Meghan Bell proposes “Broken Mirror Syndrome” as a more integrated explanation for emotional disconnection, chronic shame, and misdiagnosed narcissism, often mistaken for autism or personality disorders in adults.
I am not critiquing people with genuine neurodevelopmental conditions. I am commenting on a trend while trying to understand why there has been a massive increase in ASD and ADHD/AuDHD diagnoses and no significant change in Cluster B disorder diagnoses in the last 10 years. There has been a drift or relaxation in diagnostic criteria when it’s important to maintain diagnostic precision, in the interest of society. The growing pattern of individuals self-diagnosing with these labels and obscuring deeper interpersonal dysfunction must be examined more deeply.
Not everyone who feels socially awkward, emotionally reactive, or misunderstood is neurodivergent. Some adults exhibit antisocial or emotionally immature patterns consistent with Cluster B traits, yet choose to reframe these behaviours through the language of neurodivergence. In doing so, they position themselves as sensitive, overwhelmed, or misunderstood, rather than as individuals who might be emotionally and morally underdeveloped.
This piece focuses on adults. The diagnostic landscape for children is entirely different. I’m grateful that, at least in Australia, we have systems in place to formally assess children with suspected developmental delays. These systems not only identify support needs early but also offer remedial pathways that help children participate fully in life. They also provide guidance for parents and carers, helping them attune to their child’s developmental profile and respond with appropriate care.
This personal essay by Holly MathNerd offers a grounded, thoughtful reflection on how trauma responses, attachment disruption, and emotional neglect are often misinterpreted as signs of autism, particularly in women.
Dark neurodivergence
This piece is an invitation to think more critically about our use of diagnostic language — what it clarifies, what it protects, and what it might be obscuring — rather than a taxonomy of ADHD, autism, Cluster B, or cPTSD. I’ve linked to other writers and clinicians throughout who are also trying to make sense of this complex, shifting terrain.
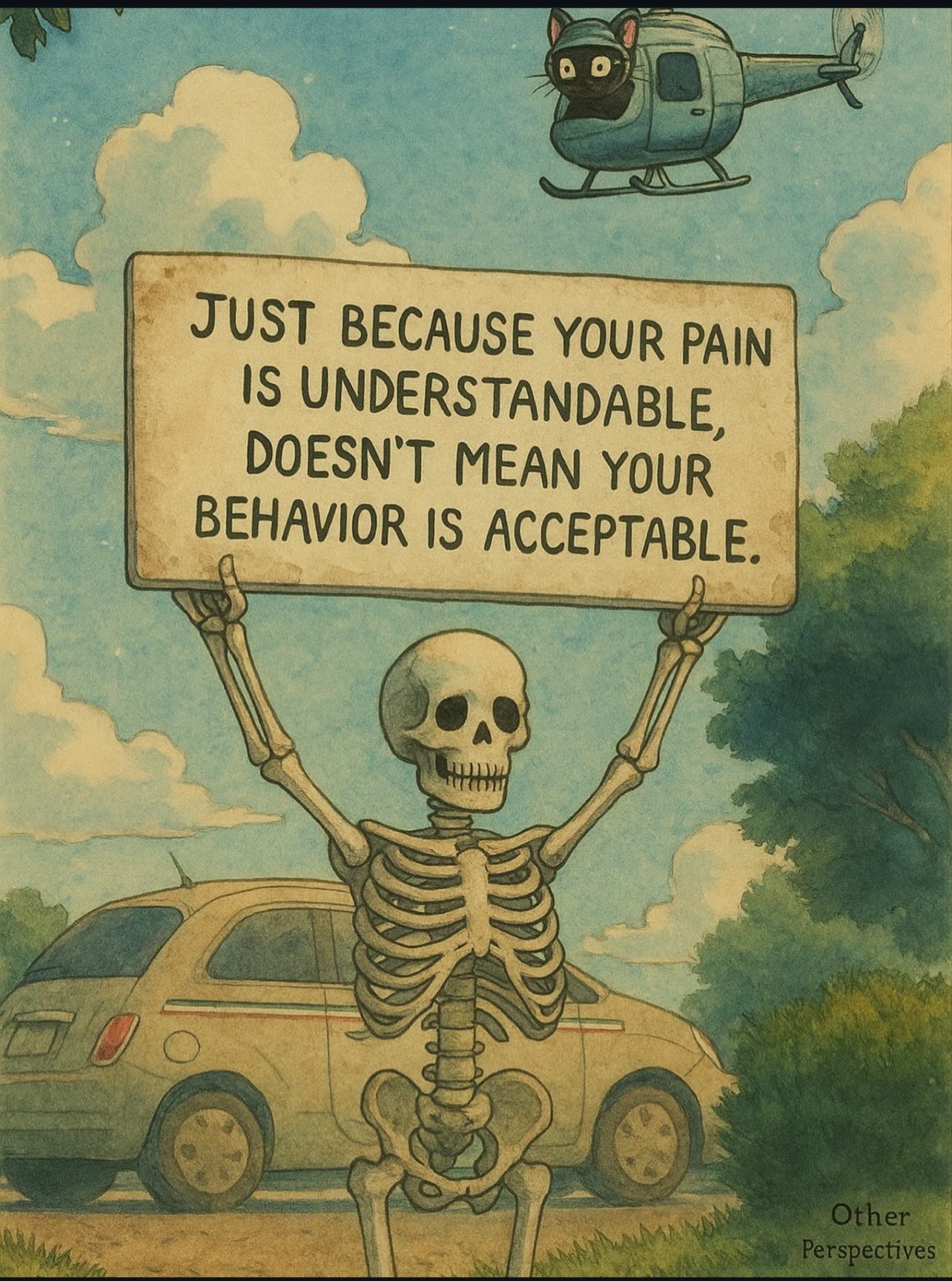
One pattern I’ve observed is what I call dark neurodivergence. This isn’t a clinical term. It’s a social pattern I’ve observed in adults who frame antisocial behaviour as trauma-based neurodivergence. These individuals often display vulnerable narcissism, covert manipulation, and antisocial tendencies that never come with real accountability. They rarely apologise unless there is something to gain. They are skilled at DARVO and consistently position themselves as the victim, the empath, and the misunderstood one. They reframe their relational dysfunction, chronic shame, fear of success, intuitive or psychic sensitivity, and spiritual inflation as symptoms of ‘neurodivergence’ rather than indicators of arrested emotional and moral development. In doing this, they protect a fragile identity while bypassing the difficult work of self-confrontation.
I can point to people who have ADHD or autism diagnoses, or who genuinely struggle with things like emotional regulation, executive dysfunction, or sensory overwhelm, but who work on themselves. They have learned to navigate relationships, to regulate themselves, and to take responsibility for their responses. The difference isn’t the label. It’s the person. Neurodivergence isn’t the problem - it’s how some people use it to shield themselves from character development and maturation. When these individuals are employed by workplaces that take their word at face value and provide accommodations without due diligence, they are inadvertently supported in facilitating the very inequitable and uncivil environments that those policies are meant to prevent.
What’s influencing the rise of dark neurodivergence
I can’t point to a single cause because this shift is coming from multiple directions: diagnostic trends1, therapy culture2, social media3, institutional policy4, and insurance frameworks5. Over the past decade, we’ve seen an increase in adult autism and ADHD diagnoses, especially among women, but no real change in the rates of Cluster B personality disorder diagnoses like BPD or NPD. It’s not due to an evolution of personality traits but more to do with the language used to describe distress has changed. What used to be recognised as emotional immaturity, unstable identity, or interpersonal dysfunction is now being explained through the language of trauma, nervous system dysregulation, neurodivergence, or systemic harm. This language removes moral weight by positioning the behaviour as accidental, automatic, or biologically determined, rather than as something the individual could take responsibility for by accessing their agency and internal locus of control.
Meghan Bell explores how childhood emotional neglect might underlie traits now often self-identified as autism, reviving aspects of the old “refrigerator mother” theory in a modern context.
This shift is reinforced by therapeutic models that centre compassion but often avoid accountability. Instead, they’ve been replaced by frames and explanations (sometimes justifications) that can over-accommodate and under-challenge. In an effort to reduce stigma, some therapists interpret nearly all behaviour through a compassionate, trauma-informed lens that avoids naming anything as problematic. Instead, behaviours are reinterpreted as protective strategies, which is not incorrect, but downplays or invalidates the harm those strategies can cause. Behaviour that clearly interferes with a person’s ability to function, relate, or regulate is met with validation, but not always with structure or intervention. The result is that some behaviours are never challenged or invited to shift, only re-labelled.
More therapists now reject the use of personality disorder diagnoses because they’re viewed as stigmatising or politically problematic, rather than having been disproven. Stepping away from evidence-based frameworks doesn’t make the patterns disappear. These are well-documented relational and emotional dysfunctions that continue to affect people’s lives, regardless of what we choose to call them6. If therapists stop using structured, research-backed diagnoses and instead use frameworks based only on social justice values, without proof those frameworks lead to meaningful healing, they can compromise the effectiveness of therapy.
When that is combined with online identity culture and workplace DEI policies that accept self-reported neurodivergence without question, we end up with a system that rewards performance over self-awareness. It’s a climate where the difference between a genuine support need and a character issue is often ignored or treated as too politically risky to touch.
Testing for ASD/ADHD instead of Cluster B
The way people are diagnosed reflects how systems are trained to respond. When someone presents with emotional volatility or interpersonal issues, they are far more likely to be assessed for autism or ADHD than for underlying character or relational dysfunction. A mix of clinical, cultural, and institutional forces shapes this pattern and steers the diagnostic process toward more acceptable and less stigmatised labels.
ASD and ADHD are palatable diagnoses
These conditions are attributed to neurological differences, not stunted moral development. “Your brain is different” sounds neutral, even sympathetic compared to the judgment-laden “your personality is disordered.” It’s easier for people to see themselves as misunderstood rather than harmful. A neurodivergent label offers access to educational and workplace accommodations, aligns with identity politics, and is protected under DEI initiatives. The label, even when self-diagnosed, explains behaviour without implicating character.Cluster B diagnoses are socially damaging
Scroll through TikTok, Instagram, Substack (including mine), or therapist content online and you’ll find a flood of warnings about narcissists and toxic people. Narcissistic traits are often framed as inherently dangerous, abusive, or beyond repair, especially when expressed by women, who are frequently branded as manipulative, crazy, or emotionally unsafe. While there is truth in these patterns in specific populations of women7, this framing makes it incredibly difficult for those who recognise narcissistic traits in themselves to seek help. Online coaches and therapists often describe NPD as untreatable, reinforcing the belief that these individuals can’t change. But as Dr. Giancarlo Dimaggio points out, most people with NPD are not sadistic - they are anxious, ashamed, and emotionally rigid. According to his clinical work, change is possible with the right therapeutic approach.
Dr. Giancarlo Dimaggio with Quillette offers a helpful corrective to this oversimplification in his interview on narcissistic personality disorder pointing out that most people with NPD are not malicious, but anxious, ashamed, and deeply self-critical.
Many therapists are hesitant to diagnose Cluster B
There are understandable reasons for this, but it’s contributing to real diagnostic drift. Some therapists avoid assigning heavily stigmatised labels for fear of alienating clients or reinforcing shame. Others are trained in activist or trauma-informed frameworks that focus on validating the client’s intent, rather than recognising the impact of their behaviour8. In many cases, therapists are simply not adequately trained, particularly those coming through programs that prioritise social justice values over clinical rigour. They might lack both the tools and the confidence to work with clients who present with manipulative, volatile, or boundary-violating behaviours. Therapist stigma also plays a role: many clinicians carry discomfort not only with the Cluster B labels themselves, but with the idea of treating people who carry those diagnoses9. This makes it harder for clients who genuinely want help to receive structured, effective support.
Psychiatrist Hannah Spier, MD explores how female-coded expressions of Cluster B pathology are often overlooked, excused, or rebranded as activism, especially when cloaked in the language of justice, victimhood, or mental health awareness.
Cultural and online influence
On social media, ADHD, autism, and AuDHD are presented as relatable, even aspirational identities. You’ll find reels and threads explaining symptoms, normalising overwhelm, or attributing difficult behaviour to executive dysfunction or sensory shutdowns. These posts invite empathy, build community, and make people feel seen. In contrast, almost no one self-identifies with Cluster B traits online. Narcissists are cast as abusers. Borderlines are seen as chaotic or unstable. There’s no room to acknowledge the spectrum of behaviours, the nuance of relational dynamics, or the possibility of meaningful rehabilitation. While many of these accusations are valid in adult-to-adult relationships (specifically excluding Cluster B parent-to-adult-child dynamics), they’re often reduced to one-directional narratives that casts one person as the perpetrator and the other as the victim. In reality, many of these dynamics are co-created, messy, and maintained by patterns on both sides. So it makes sense that people gravitate toward diagnoses that are socially protected and personally affirming rather than those that cast them as unsafe or morally compromised.
Disaffected is a psychiatric newsletter and podcast by Josh Slocum that critically examines how mental health narratives have broken. He recently hosted Dr. Hannah Spier on the rise of Cluster B traits among female professionals.
This piece isn’t about discrediting people with real neurodevelopmental conditions… it’s about asking harder questions. Why are some behaviours relabelled as disability, while others are avoided altogether? What happens when we protect identity more than we pursue integrity? And how do we stay discerning in systems that reward the right language over honest self-examination?
These are the conditions that allow dark neurodivergence to thrive. It’s a concept that aims to confront how some use clinical language to shield antisocial patterns from accountability. It also raises a deeper issue: maybe the term neurodivergence itself is too broad, too vague, too easily adopted without reflection. As Meghan Bell put it, “Neurodivergent” is a bit of a useless term because all brains are different, and people who really “diverge” from the average on multiple dimensions can diverge in all sorts of ways, good and bad.”
If you know other writers who are exploring these tensions with honesty and nuance, especially around diagnosis, identity, and accountability, I’d love to read their work so please feel free to share.
Adult ADHD and autism diagnoses have increased sharply, especially among women, while personality disorder rates, such as borderline or narcissistic PDs have remained flat. A systematic review noted a surge in adult ADHD prevalence, linked in part to DSM‑5 changes and greater awareness .
Matheiken S, Erden M, Krishnadas R, Pinto da Costa M. Adult attention-deficit hyperactivity disorder: time for a rethink? BJPsych Advances. 2024;30(5):298-302. doi:10.1192/bja.2023.54
Jones, P. B., Gearing, J., & Leibenluft, E. (2024). Trauma and personality disorders: Myths and misconceptions. Psychology Today. Retrieved from https://www.psychologytoday.com/us/blog/from-freud-to-fluoxetine/202412/trauma-and-personality-disorders-myths-and-misconceptions
Platforms like TikTok strongly influence self‑diagnosis. Studies show that less than 50% of #ADHD content aligns with clinical guidelines, but it still drives a surge in self‑identification.
Thomas, L., & Staff, N. (. (2022). Less than 50% of #ADHD TikTok content aligns with clinical criteria: Implications for self‑diagnosis among viewers. Journal of Medical Internet Research, 24(6), e12345.
Franklin, M., & Zhao, Y. (2024). The unintended consequences of embracing self‑reported neurodivergence in workplace inclusion policies. Organizational Psychology Review, 14(1), 56–72.
Across countries like the US, Canada, the UK, and Australia, systems fund ADHD and autism more readily than personality disorders . Clinicians and clients naturally gravitate toward diagnoses that unlock resources and validation.
American Psychiatric Association. (2020). Mental Health Parity and Addiction Equity Act (MHPAEA). This federal law requires health plans to provide mental health coverage that’s no more restrictive than for medical/surgical care. While ADHD and autism treatments are typically classified as medically necessary and covered, personality disorders often fall outside these allowances leaving coverage inconsistent and limited.
Smith, A. L., & Romero, L. (2025). Funding disparities across mental health diagnoses: A comparative analysis of ADHD, autism spectrum, and personality disorders in insurance claims. Health Policy & Planning, 40(3), 227–239.
This paper argues that the BPD label is gendered and dehumanising, turning women’s trauma responses into dysfunction and stripping them of context. It shows how psychiatry has historically framed women’s distress as deviance. I agree the term “borderline” is flawed, but rejecting it without a better alternative risks erasing the real relational patterns and harms some women are trying to name and understand.
Shaw, C., & Proctor, G. (2005). I. Women at the Margins: A Critique of the Diagnosis of Borderline Personality Disorder. Feminism & Psychology, 15(4), 483–490.
Post-publication reference correction: The original citation listed was an AI-generated fabrication that I mistakenly included while compiling sources for this article. This was an oversight on my part and a reminder that proofreading reference lists and double-checking sources is just as important as reviewing the written content itself. I appreciate J.D. Haltigan who kindly pointed it out. The correct reference is:
This paper looks at how women with borderline personality disorder (BPD) are judged based on how they behave and whether they’re openly diagnosed. It shows that when women show signs of BPD ie. intense emotions or unstable relationships, they often face strong stigma, including being seen as dangerous or in need of control. The reactions are shaped by gender stereotypes: women are more likely to be blamed or pitied depending on the situation, which makes it harder for them to be understood or supported.
Amestoy, M. E., Best, M. W., Ruocco, A. C., & Uliaszek, A. A. (2024). Borderline personality disorder stigma: Examining the effects of diagnostic disclosure, behavior, and gender as sources of stigma in the general population. Personality Disorders: Theory, Research, and Treatment, 15(4), 254–263.
I can access the full paper through my institutional affiliation so let me know if you'd like a copy.
Many therapists are hesitant to diagnose Cluster B traits, often avoiding these labels due to their stigma or potential to alienate clients. This reluctance is partly driven by concerns about how these diagnoses can contribute to epistemic injustice in women by framing trauma responses as pathological and undermining patients’ credibility and self-understanding.
Watts J. The epistemic injustice of borderline personality disorder. BJPsych International. 2024;21(4):78-82. Retrieved from https://www.cambridge.org/core/journals/bjpsych-international/article/epistemic-injustice-of-borderline-personality-disorder/010CBB826061A040F6537B8B8A738A41
This paper shows that BPD is one of the most stigmatised diagnoses in mental health care, with women often judged as manipulative or emotionally difficult based more on the label than their actual behaviour. These perceptions lead to reduced empathy and exclusion from care, making it harder for women who relate to these traits to seek support.
Baker, J & Beazley, P. (2022). Judging Personality Disorder: A Systematic Review of Clinician Attitudes and Responses to Borderline Personality Disorder. Journal of Psychiatric Practice, 28, 275-293.
I can access the full paper through my institutional affiliation so let me know if you'd like a copy.
Hack narcissism and support my work
I believe that a common threat to our individual and collective thriving is an addiction to power and control. This addiction fuels and is fuelled by greed - the desire to accumulate and control resources in social, information (and attention), economic, ecological, geographical and political systems.
While activists focus on fighting macro issues, I believe that activism also needs to focus on the micro issues - the narcissistic traits that pollute relationships between you and I, and between each other, without contributing to existing injustice. It’s not as exciting as fighting the Big Baddies yet hacking, resisting, overriding and deprogramming our tendencies to control others that also manifest as our macro issues is my full-time job.
I’m dedicated to helping people understand all the ways narcissistic traits infiltrate and taint our interpersonal, professional, organisational and political relationships, and provide strategies for narcissism hackers to fight back and find peace.
Here’s how you can help.
Order my book: The Little Book of Assertiveness: Speak up with confidence
Support my work:
through a Substack subscription
by sharing my work with your loved ones and networks
by citing my work in your presentations and posts
by inviting me to speak, deliver training or consult for your organisation
Hacking Narcissism is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.









This is really well done, and you know I agree that this is what's going one. Thank you for putting it out there. Many, many people know that what you're writing is true, but they will pretend they don't know it.
There's one point on which I'd add something, or perhaps disagree a bit.
You wrote:
"While there is truth in these patterns in specific populations of women6, this framing makes it incredibly difficult for those who recognise narcissistic traits in themselves to seek help."
My view? That's too bad. The behavior is stigmatized because it *deserves to be stigmatized.* Sympathy-first for the one with a personality disorder (as compared to sympathy-first for the person affected by her Cluster B behavior) is where we're already at. That's why we're here.
I don't care if the narcissist finds it "stigmatizing." I want them to find it stigmatizing. Why? Because most Cluster Bs-not all, but most-are not ever going to change. We're not going to get an appreciable number of narcissists to suddenly see themselves for who they are by "avoiding stigma."
Avoiding stigma is what has allowed Cluster Bs to normalize their behavior and to abuse with abandon. Not only are they not recognized as abusive, their abuse itself is validated and praised as "authenticity."
I care first about helping people avoid the effects of Cluster Bs, because I think that will help more people than (what I believe is) a vain hope that "offering palatable terms" will make a Cluster B suddenly realize she's the problem.
What do you think?
Thanks Nathalie. This is a thoughtful piece of work that aligns well with my clinical experience over recent years. Clinical and research understanding of personality disorders has developed massively. What we call it is a different question. But there has never been more concensus about what people with these problems need in order to function better. And one of the things they need is accountability. In a culture of identity shopping, neuro divergence and cPTSD are easier to accept or adopt as self applied labels. But diagnosistic systems are not intended to offer identity. They are intended to signpost towards help with functioning better.